About the authors: Diana Frymus is the Health Workforce Branch Chief in USAID’s Office of HIVAIDs and Jennifer Daniels is a Human Resources for Health Specialist in USAID/Southern Africa.
All over the world, health workers have demonstrated their dedication to maintaining HIV services while combating COVID-19, seeking innovative means of continuing to support clients -- from the expansion of programs that give patients three to six months’ worth of antiretroviral therapy (ART), and creating more convenient options for drug pick-up, to the use of telehealth and virtual services to support prevention and support clients in continuing their treatment. For all these innovations, the health workforce has led the charge for safely maintaining access and reach to different HIV client populations.
To recognize efforts by health care workers, The World Health Organization designated 2021 as ‘Year of the Health and Care Worker.’ Already often under-resourced and stretched thin due to staffing shortages, health workers have worked selflessly while often putting themselves at risk. For example, last year, over 400 incidents of violence against health workers were reported across the globe directly related to the COVID-19 pandemic response. While data are limited, COVID-19 infection rates among health workers have been significant. COVID-19 has highlighted the risks of insufficient and poorly trained health workers to meet patient and population needs and underscored the urgent need to ensure that healthcare workers are safe and remain healthy. 2021 is the year that health workers globally should be given improved working conditions, fair and equitable treatment, and services that support their holistic wellness and mental health.
Throughout the pandemic response, USAID has worked closely with country governments to modify how its PEPFAR-supported health workforce staffing investments have been utilized to support rapid adaptations and innovations in service delivery that have greatly enabled continued provision of HIV services. In South Africa, USAID supports more than 1,300 public health facilities across 15 high burden districts and reaches over 2.2 million people with lifesaving ART. With 1.5 million cases of COVID-19 reported since March 2020, it was imperative to mobilize resources to curb the impact of the pandemic. Support for health workers has been a critical component of the response to combat both HIV and COVID-19 and essential for maintaining morale and resilience.
As USAID joins the global community in giving gratitude to health workers as part of World Health Worker Week, we also pause to acknowledge the work that local partners have done to support and safeguard health workers highlighting examples from South Africa.
Using Virtual and Telehealth Tools to Safeguard Employees
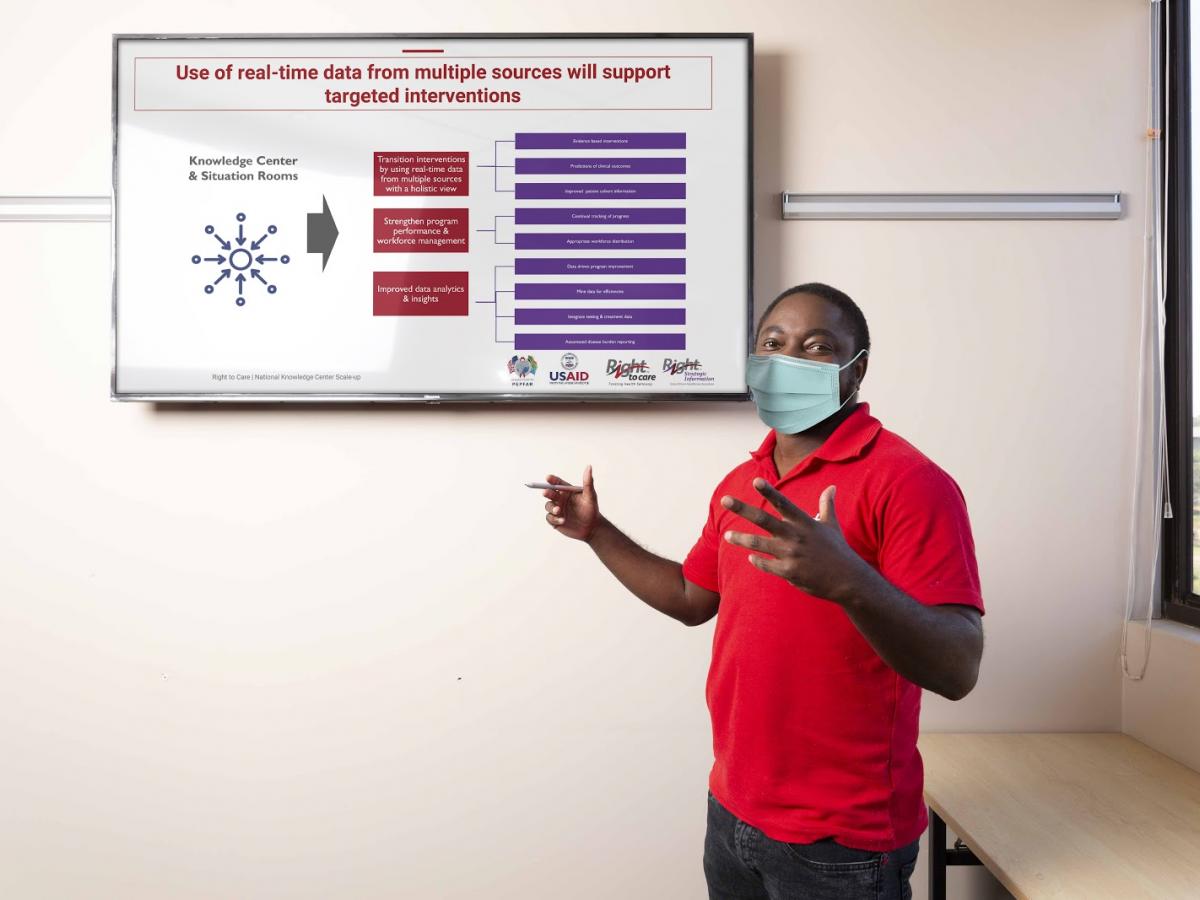
Ongoing data collection and analysis has allowed Right to Care (RTC) to assess, monitor, and swiftly respond to the needs of over 2,200 staff across South Africa. This effort was conducted under the oversight of a clinical advisory committee consisting of RTC doctors, nurses, social workers and HR managers. The USAID local partner developed a range of virtual and telehealth tools to safeguard the health and wellbeing of its employees, including a COVID-19 helpline to enable medical advisors to provide contact tracing for staff infected by the virus as well as to provide medical support. Additionally, regular video calls are held for staff to discuss personal protective equipment and use, contact tracing, and how to safely isolate or quarantine.
Using Risk Profiles to Protect the Vulnerable and High-Risk
Recognizing the greater risks faced by its vulnerable employees, Maternal, Adolescent, and Child Health Institute (MatCH) moved quickly to identify staff that were most at-risk of severe reactions to COVID-19 exposure to make accommodations for those that were patient-facing. These risk profiles identified almost a third of MatCH’s professional nurses were over the age of 55, with a comorbidity. To reduce their risk of exposure, these nurses shifted from seeing clients in person to providing virtual support to facilities. Virtual support included generating patient appointment lists and auditing files, providing telephonic consultations to clients, and assisting with pre-packaging of medication and arranging medicine pick-ups for HIV clients. These revision of duties has ensured continued provision of HIV services while also reducing risk of exposure to COVID-19.
Providing Psychosocial and Mental Health Support
Partners identified that a high proportion of staff were experiencing exhaustion, stress, and anxiety due to the pandemic and that there was a need to provide additional psychosocial support and access to mental health services. Anova designed a weekly Wellness workshop to help staff deal with mental and emotional issues while living and working through a pandemic. Additionally, a group of mental health practitioners provided psychosocial support to staff affected by COVID-19. Wits RHI also provided online support services, as well as deployed in-house psychologists and social workers to enhance staff support. RTC developed an e-learning course for health workers to manage mental resilience and employ wellness practices; 3,437 healthcare workers are enrolled on the mental health resilience course.
With hope on the horizon for combatting COVID-19, the pandemic has underscored the importance of a resilient health workforce, and the need to build capacity for health worker safeguarding and support as part of health workforce investments and interventions. A well equipped, safe, and healthy workforce can respond not only to emerging threats, but also adequately maintain essential services.
